Stress is often described as something that lives only in the mind, but the body feels it too. For people with menstrual cycles, stress can show up in subtle or noticeable ways, sometimes affecting timing, symptoms, or how a cycle feels overall. Understanding this connection can bring clarity without placing blame or pressure on the person experiencing it.
Stress-related cycle changes are not a sign of failure or poor coping. They are a reflection of how closely the body’s systems are connected.
How Stress Shows Up in Your Cycle
Stress as a whole-body experience
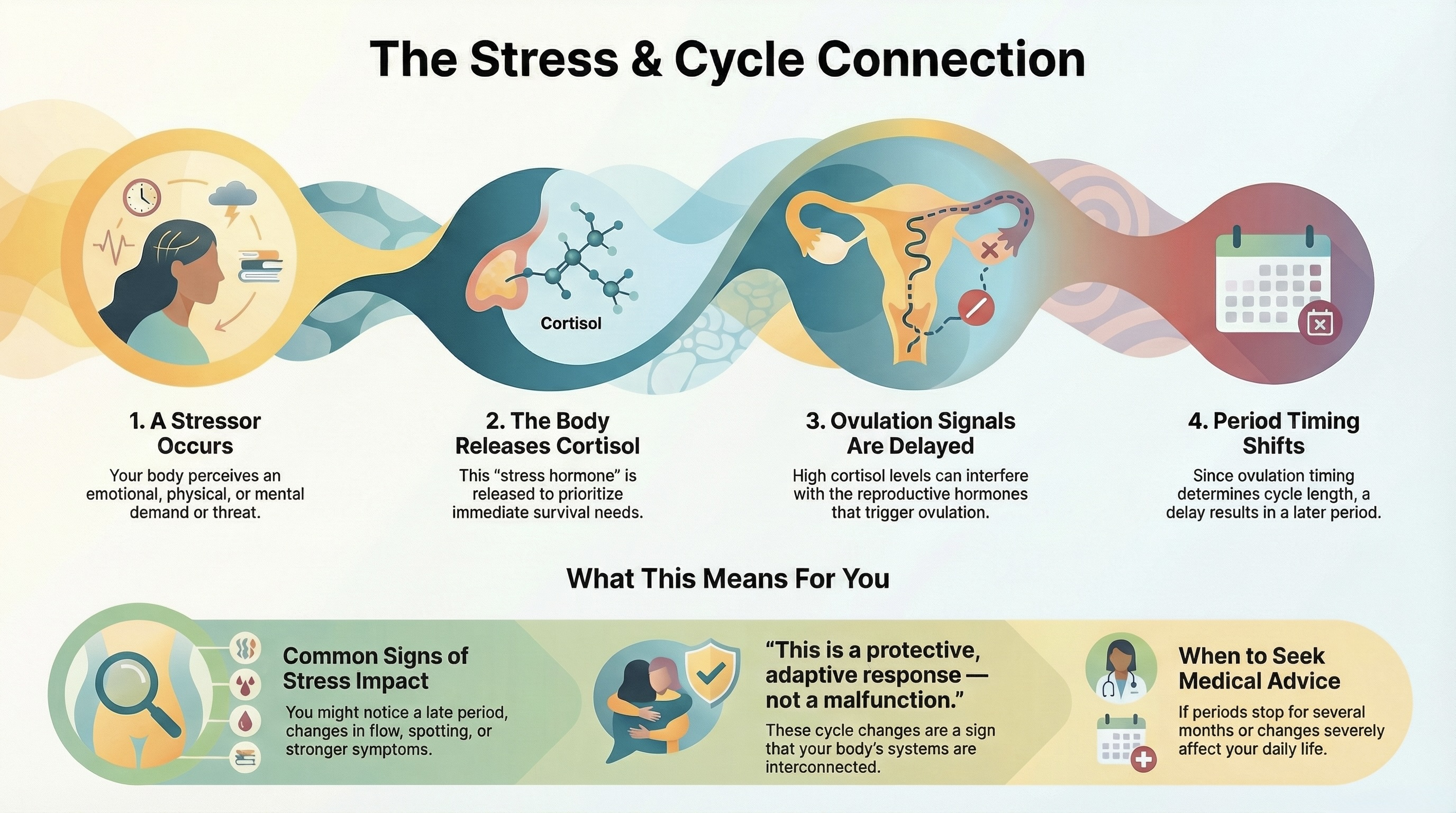
Stress is the body’s response to perceived demands or threats. It can come from emotional situations, mental load, physical illness, lack of sleep, major life changes, or ongoing responsibilities. The body responds by releasing hormones designed to help it cope.
One of these hormones is cortisol. Cortisol plays an important role in helping the body respond to challenges. It affects energy use, alertness, and immune function. Cortisol does not exist in isolation — it interacts with many other hormones, including those involved in the menstrual cycle.
This interaction is where stress can begin to influence cycle patterns.
Cortisol and reproductive hormones
Reproductive hormones like estrogen and progesterone follow a repeating rhythm across the menstrual cycle. This rhythm is guided by signals between the brain and the ovaries.
Cortisol can influence these signals. During times of stress, the body may prioritize immediate survival needs over longer-term processes like reproduction. This does not mean reproduction is “turned off,” but it can mean timing shifts.
When cortisol levels are elevated, the signals that trigger ovulation can be delayed. Since ovulation plays a major role in determining cycle length, a delay can result in a longer cycle or a later period.
This is a protective, adaptive response — not a malfunction.
Why stress can delay ovulation
Ovulation does not happen on a fixed calendar date. It occurs when hormone signals align. Stress can temporarily change how quickly those signals build.
A stressful event, whether emotional or physical, can slow down the body’s readiness to ovulate. This might happen during intense work periods, illness, travel, grief, or sustained mental load.
When ovulation is delayed, the period that follows is also delayed. This can feel confusing or alarming, especially if cycles are usually regular. In many cases, once stress levels shift, the cycle returns to its usual pattern.
Short-term versus long-term stress effects
Short-term stress often leads to temporary changes. A single late period, a skipped ovulation, or an unusually long cycle can happen during a particularly stressful month. These changes often resolve on their own.
Long-term or chronic stress can have more ongoing effects. Over time, repeated stress responses may contribute to more frequent cycle irregularity, changes in symptoms, or shifts in how periods feel.
Importantly, not everyone responds to stress in the same way. Two people under similar pressure may see very different cycle effects. This variability is normal.
Common experiences people notice
People often notice cycle changes during stressful periods of life. Periods may arrive later than expected, symptoms may feel stronger, or cycles may feel less predictable.
Some notice more spotting, changes in flow, or differences in how their body feels before or during a period. Others notice emotional or energy changes tied to stress rather than bleeding patterns.
It is also common for cycles to feel “off” during times of transition and then settle again later.
What is generally considered normal
Occasional cycle changes during stressful times are common. A delayed period, a longer cycle, or a month with different symptoms can fall within normal patterns, especially when linked to identifiable stressors.
Normal includes cycles that adapt to life circumstances and then return to baseline. It also includes variability — not every stressor leads to a noticeable change, and not every change has an obvious cause.
Stress-related cycle shifts do not require perfection or constant control to be considered healthy.
Compassionate framing matters
It is common to hear messages that imply stress-related cycle changes are something a person should fix by “managing stress better.” This framing can feel unrealistic or blaming, especially when stress comes from unavoidable life demands.
Stress responses are not choices. They are automatic physiological processes. Recognizing how stress shows up in the cycle is about understanding, not correction.
Awareness can help replace self-criticism with compassion.
When it can make sense to seek medical advice
Medical advice can be helpful when cycle changes persist over many months, occur without any identifiable life changes, or are accompanied by other concerning symptoms.
Periods that stop for several months, cycles that become consistently very irregular, or changes that significantly affect daily life may be worth discussing with a healthcare professional.
Seeking guidance is about gaining clarity and support, not about assuming stress is the sole cause.
A calm conclusion
Stress and the menstrual cycle are connected because the body is an integrated system. Cortisol can interact with reproductive hormones, sometimes delaying ovulation and shifting cycle timing. These changes are adaptive responses, not personal failures.
Understanding how stress shows up in the cycle — without blame or pressure — can help reduce anxiety and build trust in the body’s ability to respond and recover.